Your voice isn’t just how you speak, it’s how you connect, express yourself, and show up in the world. When that voice is affected by cancer treatment, surgery, illness, or ongoing strain, it can feel like you’ve lost a part of yourself.
We’re here to help you get it back.
Our voice therapy program is designed to treat a wide range of conditions, including:
Muscle Tension Dysphonia: when tightness or poor vocal coordination alters voice quality or makes speaking exhausting
Vocal Cord Dysfunction (VCD): often mistaken for asthma, this affects breathing and voice during activity or stress
Chronic Cough: persistent, non-productive coughing that doesn’t respond to medication and disrupts daily life
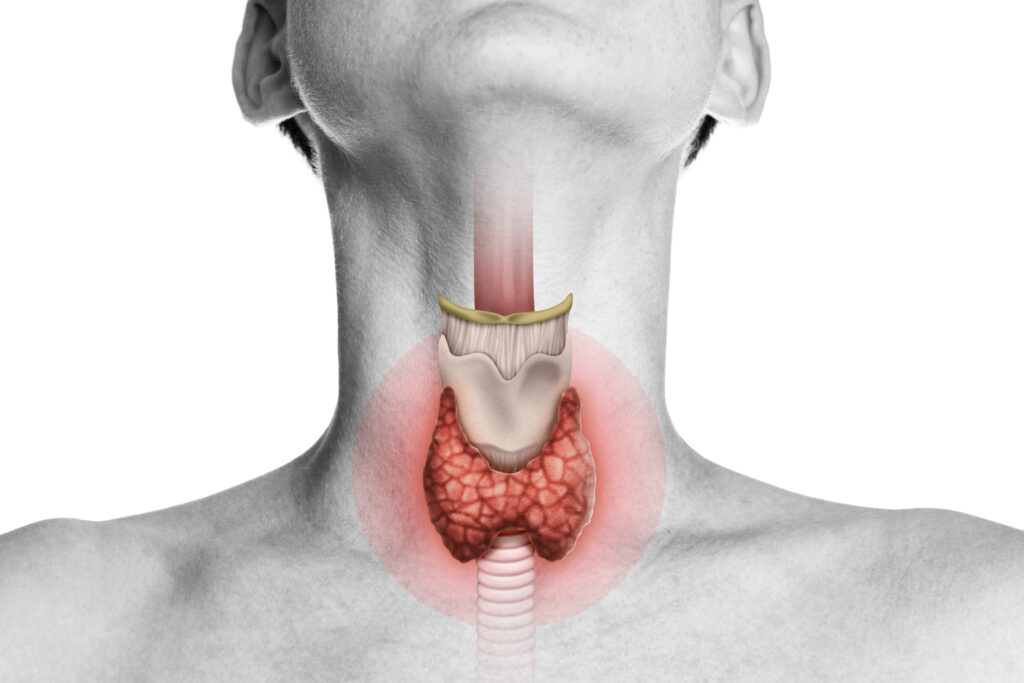
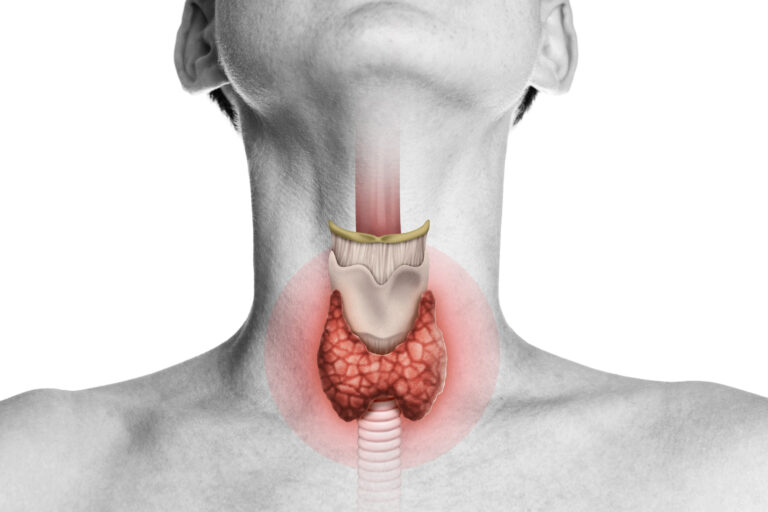
For patients undergoing or recovering from cancer treatment, especially head and neck cancers, thyroid surgeries, or radiation near the airway, voice therapy can play a critical role in protecting, restoring, and strengthening vocal function. Whether you’re preparing for treatment, navigating the side effects mid-process, or working to recover after surgery or radiation, we tailor therapy to your timeline, diagnosis, and goals.
Treatment includes voice retraining, breathing coordination, vocal hygiene strategies, and techniques to reduce strain and restore clarity. It’s personalized, practical, and built around what your voice needs to feel strong, sustainable, and heard.